Learn everything you need to know about type 2 diabetes—from early symptoms and causes to natural treatments, lifestyle tips, and expert-approved management tools. Take control of your health today.
Table of Contents
What Is Type 2 Diabetes?
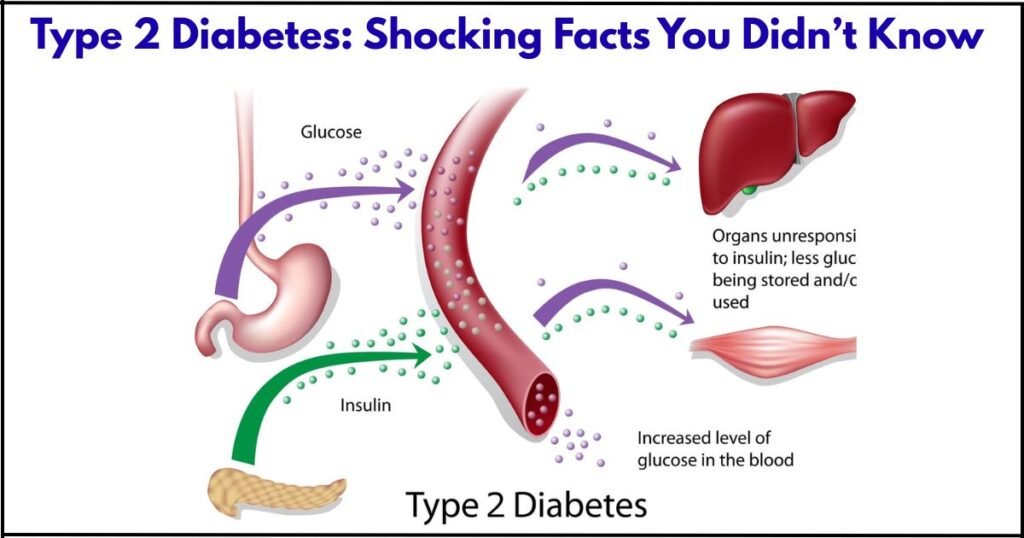
Type 2 diabetes is a chronic health condition that affects how your body processes blood sugar (glucose). In people with type 2 diabetes, the body either doesn’t produce enough insulin or becomes resistant to it. Insulin is the hormone that helps move glucose from your bloodstream into your cells, where it’s used for energy.
When insulin isn’t working properly, glucose builds up in the blood. Over time, high blood sugar levels can lead to serious health issues like heart disease, kidney damage, nerve problems, and vision loss. Unlike type 1 diabetes, which usually develops early in life and requires insulin therapy from the start, type 2 diabetes often develops in adults and may initially be managed with lifestyle changes.
This condition is strongly linked to factors like being overweight, physically inactive, over 45 years old, or having a family history of diabetes. However, more young people—including teens and children—are being diagnosed due to rising obesity rates and poor diet.
With early diagnosis and the right care, type 2 diabetes can be effectively managed—and in some cases, even reversed through healthy lifestyle changes.
Early Signs and Symptoms!
Recognizing the early signs of type 2 diabetes is crucial for timely treatment and preventing complications. In the early stages, many people don’t notice any symptoms because blood sugar levels rise gradually over time. However, your body does give warning signals that shouldn’t be ignored.
Common Early Symptoms
- Frequent urination – High blood sugar causes your kidneys to work overtime to remove excess glucose, leading to more trips to the bathroom—especially at night.
- Increased thirst – As you lose more fluids through urination, your body becomes dehydrated, triggering constant thirst.
- Unusual hunger – Because your cells aren’t getting enough glucose for energy, you may feel hungry even after eating.
- Fatigue and weakness – When glucose can’t enter cells effectively, your body lacks energy, leaving you feeling tired and sluggish.
- Blurry vision – Rising blood sugar can cause swelling in the eye lenses, leading to temporary vision changes.
- Slow-healing wounds – Cuts or sores that take longer to heal may signal poor blood flow and nerve damage caused by type 2 diabetes.
- Tingling or numbness – A burning or tingling sensation in hands and feet can indicate early nerve damage (diabetic neuropathy).
- Dark patches on the skin – Areas of darkened, velvety skin—usually around the neck or armpits—can be a sign of insulin resistance, a key factor in type 2 diabetes.
- Unexplained weight loss or gain – Some people lose weight because their bodies can’t use glucose properly, while others gain due to insulin imbalance.
Why Early Detection Matters
Catching type 2 diabetes early gives you the best chance to control it through healthy eating, exercise, and medication if needed. Delayed diagnosis increases the risk of serious complications like heart disease, kidney problems, and nerve damage.
Causes and Risk Factors
Type 2 diabetes develops when your body becomes resistant to insulin or when the pancreas doesn’t produce enough insulin to keep blood sugar levels in check. While the exact cause isn’t fully understood, several key factors significantly increase the risk.
Main Causes of Type 2 Diabetes
- Insulin resistance: In many people, cells in the muscles, liver, and fat stop responding properly to insulin. As a result, glucose stays in the bloodstream instead of entering the cells for energy.
- Pancreatic dysfunction: Over time, the pancreas may become unable to keep up with the body’s increased insulin needs, leading to rising blood sugar levels.
- Chronic inflammation: Low-level inflammation caused by excess fat and poor diet may also contribute to insulin resistance and beta-cell damage in the pancreas.
- Genetics: A family history of type 2 diabetes increases your risk, especially if a close relative has the condition.
Top Risk Factors for Developing
- Being overweight or obese – Excess fat, especially around the abdomen, contributes to insulin resistance.
- Lack of physical activity – Sedentary lifestyles reduce the body’s ability to use insulin effectively.
- Age 45 or older – Risk increases with age, although younger people—including children—are now being diagnosed more frequently.
- Family history – Having a parent or sibling with type 2 diabetes raises your chances.
- Poor diet – High intake of processed foods, sugar, and refined carbs raises blood sugar levels over time.
- High blood pressure or cholesterol – These metabolic issues often occur together with insulin resistance.
- Gestational diabetes – Women who had diabetes during pregnancy are at greater risk later in life.
- Polycystic ovary syndrome (PCOS) – This hormonal disorder is associated with insulin resistance.
- Ethnicity – People of South Asian, African, Hispanic, and Native American descent are at higher risk.
Type 2 Diabetes vs. Type 1 Diabetes: Key Differences Explained
While both type 2 diabetes and type 1 diabetes affect how the body regulates blood sugar (glucose), they are very different in terms of causes, age of onset, and treatment.
Understanding the differences is important for managing the condition properly and avoiding confusion.
Type 2 Diabetes
- Cause: The body becomes resistant to insulin or doesn’t make enough insulin.
- Onset: Usually develops in adults over 45, but is increasingly seen in younger people due to obesity and poor diet.
- Progression: Gradual—often starts with mild symptoms or none at all.
- Treatment: Often managed with lifestyle changes (diet and exercise), oral medications, and sometimes insulin.
- Reversible?: In early stages, it may be reversed or put into remission through lifestyle changes.
Type 1 Diabetes
- Cause: An autoimmune condition where the body’s immune system attacks insulin-producing cells in the pancreas.
- Onset: Typically begins in childhood or adolescence, though it can appear in adults.
- Progression: Rapid—symptoms appear suddenly.
- Treatment: Requires daily insulin injections or use of an insulin pump for life.
- Reversible?: No. It cannot be prevented or cured.
Comparison Table: Type 2 vs. Type 1 Diabetes
| Feature | Type 2 Diabetes | Type 1 Diabetes |
|---|---|---|
| Cause | Insulin resistance / reduced insulin | Autoimmune destruction of insulin cells |
| Usual Onset Age | Adults over 45 (but increasing in youth) | Childhood or early teens |
| Speed of Onset | Gradual | Sudden |
| Insulin Required? | Sometimes | Always |
| Preventable? | Often with healthy habits | No |
| Reversible? | Sometimes through diet/lifestyle | No |
How Is Type 2 Diabetes Diagnosed?
Diagnosing type 2 diabetes is done through simple blood tests that measure your blood sugar levels. If you’re experiencing symptoms like frequent urination, excessive thirst, or fatigue—or if you’re at risk—it’s important to get tested early.
Doctors typically use one or more of the following tests to confirm a type 2 diabetes diagnosis:
1. A1C Test (Hemoglobin A1C)
- What it does: Measures your average blood sugar levels over the past 2–3 months.
- Normal: Below 5.7%
- Prediabetes: 5.7% to 6.4%
- Type 2 diabetes: 6.5% or higher (on two separate tests)
✅ This is the most common and convenient test, often done without fasting.
2. Fasting Blood Sugar Test (FBS)
- What it does: Measures blood sugar after you haven’t eaten for at least 8 hours.
- Normal: Less than 100 mg/dL
- Prediabetes: 100–125 mg/dL
- Type 2 diabetes: 126 mg/dL or higher (confirmed with a repeat test)
3. Oral Glucose Tolerance Test (OGTT)
- What it does: Measures your body’s response to sugar after drinking a glucose solution.
- Normal: Less than 140 mg/dL after 2 hours
- Prediabetes: 140–199 mg/dL
- Type 2 diabetes: 200 mg/dL or higher after 2 hours
📝 This test is often used for pregnant women or when other results are unclear.
4. Random Blood Sugar Test
- What it does: Measures blood sugar at any time, regardless of when you last ate.
- Result: 200 mg/dL or more with symptoms may indicate type 2 diabetes.
What Happens After Diagnosis?
If you’re diagnosed with type 2 diabetes, your doctor may recommend lifestyle changes, medications, or additional tests to monitor your condition. Early detection helps you manage the disease and avoid complications like nerve damage, kidney issues, or vision loss.
Treatment Options
Managing type 2 diabetes involves a combination of lifestyle changes, medications, and regular monitoring to keep blood sugar levels in a healthy range. Treatment plans vary depending on your age, health status, and how long you’ve had the condition.
1. Lifestyle Changes
- Healthy eating: Focus on whole grains, lean proteins, vegetables, and foods low in sugar and saturated fats. Portion control is key.
- Regular exercise: Aim for at least 30 minutes of moderate activity (like walking or cycling) five days a week to improve insulin sensitivity.
- Weight loss: Losing even 5–10% of your body weight can significantly improve blood sugar control.
2. Oral Medications
- Metformin is usually the first medication prescribed for type 2 diabetes. It helps your body use insulin more effectively.
- Other medications may stimulate insulin production or reduce sugar absorption from food.
3. Insulin Therapy
- Some people may eventually need insulin if oral medications and lifestyle changes are not enough.
- Insulin is injected and helps lower blood sugar quickly and effectively.
4. Continuous Monitoring
- Regular A1C tests and daily blood sugar checks help track your progress and guide treatment adjustments.
With the right approach, many people with type 2 diabetes can live healthy, active lives.
Best Foods for Type 2 Diabetes: What to Eat and Avoid
Eating the right foods is one of the most effective ways to manage type 2 diabetes. A balanced diet helps stabilize blood sugar, improve energy, and reduce the risk of complications.
Best Foods to Eat
- Leafy greens: Spinach, kale, and broccoli are low in carbs and rich in fiber.
- Whole grains: Brown rice, quinoa, and oats have a low glycemic index and keep you full longer.
- Lean proteins: Skinless chicken, fish, eggs, tofu, and legumes help build muscle without spiking blood sugar.
- Healthy fats: Avocados, nuts, and olive oil support heart health.
Foods to Avoid
- Sugary drinks: Soda, energy drinks, and sweetened coffee can cause rapid blood sugar spikes.
- Refined carbs: White bread, pastries, and processed snacks are high in empty calories.
- Fried and fatty foods: These can worsen insulin resistance and raise cholesterol.
- High-sugar desserts: Cakes, candies, and ice cream should be limited or replaced with healthier alternatives.
Making mindful food choices is essential for anyone living with type 2 diabetes.
Exercise Tips for Managing
Regular physical activity plays a key role in managing type 2 diabetes. Exercise helps lower blood sugar, improves insulin sensitivity, supports weight loss, and boosts overall energy and mood.
Top Exercise Tips
- Start with walking
A 30-minute brisk walk five days a week is a simple and effective way to get moving. It’s easy on the joints and doesn’t require any equipment. - Mix in strength training
Try light weights, resistance bands, or bodyweight exercises (like squats or push-ups) 2–3 times per week. Strength training builds muscle, which helps the body use glucose more efficiently. - Stay consistent
Schedule your workouts like appointments. Even 10-minute sessions throughout the day can make a difference. - Check blood sugar levels
Monitor your blood glucose before and after exercise to learn how your body responds. - Stay hydrated and wear proper shoes
Drink water and choose supportive footwear to avoid injury—especially important for those with diabetic foot concerns.
Staying active is one of the most powerful tools for living well with type 2 diabetes.
Can You Reverse Type 2 Diabetes Naturally?
The short answer is: yes, in some cases, type 2 diabetes can be reversed naturally—especially if it’s caught early. Reversing doesn’t mean the condition is cured forever, but it means your blood sugar levels can return to a healthy range without the need for medication.
How Natural Reversal Works
- Weight loss: Losing even 5–10% of your body weight can drastically improve insulin sensitivity.
- Low-carb, balanced diet: Focusing on whole foods, fiber, and healthy fats helps stabilize blood sugar.
- Regular exercise: Daily physical activity boosts your body’s ability to use insulin effectively.
- Stress reduction: Chronic stress can spike blood sugar—so managing it with mindfulness, sleep, or yoga helps.
- Consistent habits: Natural reversal takes commitment and long-term changes in diet and lifestyle.
However, not everyone can reverse type 2 diabetes, especially if it’s been present for many years. But even if reversal isn’t possible, these changes still improve blood sugar control and overall health.
Complications of Uncontrolled
If type 2 diabetes is not properly managed, high blood sugar over time can damage many parts of the body. These complications can be serious—even life-threatening—but most are preventable with early action and good blood sugar control.
Common Complications
- Heart disease and stroke
People with type 2 diabetes are at higher risk of heart attacks, high blood pressure, and strokes due to damaged blood vessels. - Kidney damage (diabetic nephropathy)
High blood sugar can weaken the kidneys over time, potentially leading to kidney failure or dialysis. - Nerve damage (diabetic neuropathy)
Tingling, numbness, or pain—especially in the hands and feet—is common and may lead to serious infections. - Eye damage (diabetic retinopathy)
If left untreated, type 2 diabetes can lead to vision loss or blindness. - Foot problems
Reduced circulation and nerve damage increase the risk of foot ulcers, infections, and in severe cases, amputation. - Skin infections and slow healing
High blood sugar impairs your body’s ability to fight infection and repair tissue.
Managing type 2 diabetes early helps avoid these complications and leads to a healthier, longer life.
Living with Type 2 Diabetes: Daily Habits & Lifestyle Changes
Living with type 2 diabetes means making consistent lifestyle choices that support healthy blood sugar levels. These daily habits can help you feel better, reduce the need for medication, and prevent long-term complications.
Healthy Daily Habits
- Balanced meals
Eat at regular times and include fiber-rich foods, lean proteins, and healthy fats. Avoid skipping meals, as this can cause spikes or drops in blood sugar. - Stay active
Aim for at least 30 minutes of exercise most days. Walking, yoga, or swimming are great low-impact options. - Monitor blood sugar
Track your glucose levels daily to understand how food, activity, and stress affect your body. - Hydration and sleep
Drink plenty of water and aim for 7–8 hours of quality sleep to support your overall health. - Stress management
Practice mindfulness, deep breathing, or hobbies to keep stress in check—it can impact blood sugar levels.
Making small, sustainable changes can make living with type 2 diabetes easier and more empowering.
Best Apps and Tools to Manage
Managing type 2 diabetes is easier than ever with the help of digital tools. From tracking blood sugar to planning meals, these apps and devices help you stay on top of your health—right from your smartphone.
Top Diabetes Management Apps
- MySugr
A user-friendly app that tracks blood sugar, meals, medication, and activity. It offers fun challenges and a built-in diabetes coach. - Glucose Buddy
Perfect for logging glucose readings, meals, and medications. You can generate reports to share with your doctor. - Carb Manager
Helps you monitor carbs, which is key for people with type 2 diabetes. It includes meal planning and macro tracking. - BlueStar Diabetes
Offers personalized guidance and real-time tips based on your data. FDA-approved and ideal for ongoing support.
Useful Devices
- Continuous Glucose Monitors (CGMs): Like Dexcom or FreeStyle Libre, provide real-time blood sugar trends.
- Smart glucometers: Sync with apps to simplify tracking.
These tools make living with type 2 diabetes more manageable and help you make informed choices every day.
Type 2 Diabetes in Children and Teens
Although once considered an adult condition, type 2 diabetes is now increasingly diagnosed in children and teens. This rise is largely due to poor diet, lack of physical activity, and increasing rates of childhood obesity.
Why It Happens
In young people, type 2 diabetes develops when the body becomes resistant to insulin or doesn’t produce enough. Risk factors include being overweight, having a family history of diabetes, and living a sedentary lifestyle.
Common Signs to Watch For
- Frequent urination
- Increased thirst
- Unexplained weight loss
- Fatigue
- Dark patches of skin (often around the neck or armpits)
Since symptoms can be mild or mistaken for other issues, routine check-ups are essential—especially for at-risk children.
Treatment and Management
Type 2 diabetes in children is often managed with healthy lifestyle changes like improved diet, regular exercise, and weight management. In some cases, medication may be required.
With early diagnosis and proper care, children and teens with type 2 diabetes can live healthy, active lives.
Frequently Asked Questions (FAQs) About Type 2 Diabetes
1. Can type 2 diabetes go away completely?
In some cases, especially with early diagnosis, type 2 diabetes can be reversed through weight loss, healthy eating, and exercise. However, it’s not considered a permanent cure, and ongoing management is essential.
2. What is the normal blood sugar range for someone with type 2 diabetes?
A target blood sugar level is usually:
- Before meals: 80–130 mg/dL
- 2 hours after meals: Less than 180 mg/dL
Always follow your doctor’s specific recommendations.
3. Can you drink alcohol with type 2 diabetes?
Yes, in moderation. Choose low-sugar options and avoid drinking on an empty stomach. Always check how alcohol affects your blood sugar.
4. Is type 2 diabetes genetic?
Genetics can increase your risk, especially if a parent or sibling has it. But lifestyle factors also play a major role.
5. Do you need insulin for type 2 diabetes?
Not always. Many people manage with diet, exercise, and oral medication. Insulin may be needed if blood sugar remains uncontrolled.
Conclusion: Managing and Thriving with Type 2 Diabetes
Living with type 2 diabetes may seem overwhelming at first, but with the right tools, knowledge, and daily habits, it’s absolutely possible to live a full, healthy life. The key is consistent management—through balanced nutrition, regular physical activity, stress control, and proper medical care.
By monitoring your blood sugar levels, staying informed, and making small but powerful lifestyle changes, you can reduce your risk of serious complications and even improve or reverse the condition in its early stages. Technology, like diabetes apps and smart glucose monitors, can also make day-to-day management easier and more effective.
Support from family, friends, and healthcare professionals plays a big role in your success. Don’t be afraid to ask questions, seek advice, or join a support group.
Remember, type 2 diabetes doesn’t define you—it’s just one part of your health journey. With the right mindset and approach, you can not only manage diabetes but truly thrive.
Read the blog post best protein powder for diabetics